That might sound a little harsh but if you have symptoms of either diarrhea or constipation (or both), bloating, occasional (or chronic) abdominal pain on a somewhat regular basis you could be diagnosed with “IBS.” The only real helpful part of this diagnosis is that it means they have ruled out other, potentially more harmful conditions like IBD, Celiac, or Crohn’s disease, for example. Otherwise, it’s just telling you what you already know!
Because what does IBS actually mean? You go to the doctor because you are experiencing symptoms of your bowels being….irritable, and your doctor confirms that your bowels are…irritable. Okay, thanks?
Not helpful.
IBS is just a list of symptoms and when you have a few of them you get labeled with the diagnosis of irritable bowel syndrome.

Once you receive a diagnosis, the assumption is you’ve found the problem and can start treating it. But just being told you have IBS isn’t actually finding the problem – you already knew your bowels were “irritable!” Maybe you’re prescribed a medication to help with diarrhea or constipation. You might (hopefully) be tested for Celiac Disease and have some other blood work done. If your doctor is on top of things you may have a breath test done to check for SIBO (small intestinal bacterial overgrowth).
But what tends to be lacking is looking into WHY you are experiencing the symptoms that have gotten you that diagnosis of IBS. There’s generally a reason why this is happening. If we don’t try to address that reason, you’re always just going to be trying to play symptom control whack-a-mole.
It’s unlikely that your gut is just acting out for no reason. Our bodies are hard-wired to survive. So when we experience any kind of negative health symptom, that is just a sign that something isn’t working properly.
Wouldn’t it make more sense to try to address the body as a whole and help allow all your systems to work properly instead of just trying to attack a particular symptom? Often times when we address specific symptoms, we may quiet that one but something else pops up. Hence the whack-a-mole.
Let’s say you’ve been dealing with bloating. You start the morning out with a relatively flat stomach. By the evening, whether you’ve eaten a lot or not, you have a belly that looks like you’re 6 months pregnant. This is usually also combined with some diarrhea, constipation, or a mix of the two. Maybe not every day but often several times per week.
Your doctor may prescribe something to reduce diarrhea. But by taking a drug to make it stop you’re still not getting to the reason why it’s happening in the first place. That probably isn’t going to help the bloating.
If you’ve been diagnosed with IBS you can probably assume there is some level of malabsorption of nutrients. So even if you take medicine to stop the diarrhea you’re not addressing the fact that your body isn’t absorbing the nutrients in the food you’re eating.
Down the road that could lead to inflammation, poor bone health, memory problems, brain fog, fatigue, hormone imbalances, mental health struggles, and a million other things. Our cells that make up our bodies NEED these nutrients so if your irritable bowel isn’t absorbing them – even if you stop the diarrhea (or constipation) – it doesn’t mean you’re now absorbing your food well.
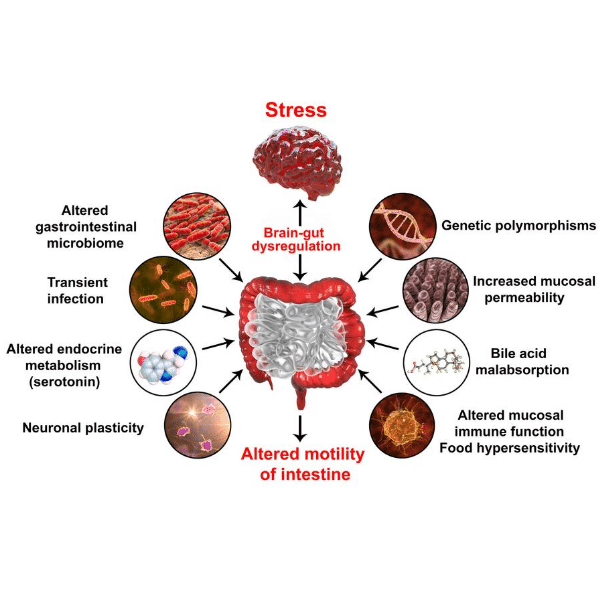
Reasons for IBS
Our bodies are so complex and there are so many things that affect our health. The gut is a complex system consisting of various hormones, glands, enzymes, gastric juices, and various processes relying on the proper functioning of whatever comes before it to be working properly. When something in the chain is showing signs of not working, we have to look at the processes above it to figure out why.
For example, let’s take constipation. (Side note – you should be having a bowel movement everyday, otherwise you are experiencing some level of constipation). Just looking at where that’s happening specifically – in your colon – doesn’t necessarily help us find relief long term. So we have to look at what’s happening before the digested food even gets to the colon. You’ve got your small intestine, the duodenum (which is part of the small intestine where the gallbladder and pancreas both send in digestive aids like bile and enzymes), the stomach, the esophagus, and the mouth. And while not part of the digestive system per-se, we have the brain which IS controlling the process.
So, if you have constipation, you may be told to take a fiber supplement. This may help, but it also just may make things worse. We should instead be asking…
- Are you hydrated?
- Do you have sufficient stomach acid production to kill off bad pathogens, break down your food into small particles so it can be absorbed, trigger the proper release of pancreatic enzymes, bile from the gallbladder, and to even just open the valve at the base of the stomach?
- Are you actually chewing your food well? This simple step can make all the difference
- Are you perpetually stressed, rushed, anxious? This will prevent your body from getting the proper message from your brain to produce enough stomach acid and gastric juices to do the important work they need to do.
- Are you eating foods that are damaging the lining of your gut?
So, you see, you can take a medicine to try to help with the specific symptom of constipation and try to speed up the transit time but that doesn’t mean you are going to help your body digest better or absorb more nutrients.
Sometimes, yes, we do need to take supplements to help with specific symptoms WHILE ALSO working on the process and system as a whole.
Being constipated means that your body is going to reabsorb toxins that it is trying to get rid of so we do want to get rid of that symptom. But we don’t want to just do that and forget about getting to the bottom of WHY it’s happening in the first place.
If you have diagnosed or symptoms of IBS, it’s important to try to get to the bottom of it. Just because you’ve been dealing with it for a long time doesn’t mean it’s “normal.” It’s certainly not ideal and speaking from experience, not fun to live with! It can also lead to more serious issues that you wouldn’t necessarily attribute to IBS.
We have to get away from the idea that our bodies are a collection of parts and that issues in the body are just issues with that particular organ, gland, or system. IBS is effecting the way your body digests. Like I mentioned above, if you’re not digesting well, you’re not absorbing your nutrients well. If you don’t absorb nutrients you won’t get what your body needs to build healthy cells.
Some consequences of IBS
When your body doesn’t get what it needs it could respond in any number of ways. Your metabolism could slow down (increase weight gain), you won’t get the vitamins and minerals needed for healthy blood sugar and insulin response (increased risk of insulin resistance, diabetes, weight gain), your hormones won’t have the building blocks they need (hormone imbalance issues), your brain won’t get the nutrition it needs (memory, concentration issues), your heart won’t get the nutrients it needs, your muscles won’t either (fatigue, muscle weakness), your bones and joints won’t get what they need, and the list goes on.
When I work with someone who (like I have!) is dealing with symptoms of IBS, I look at the digestive process as a whole, and work to optimize the functioning of the whole process. That means taking a top-down approach that looks a bit like this:
- Starting with the brain. Is she allowing her brain to tap into the parasympathetic nervous system where proper digestion actually happens? If not, we look at ways to help that take place
- Chewing / eating slowly enough. If she is on the run and wolfing down food, digestion just isn’t going to happen ideally.
- Ensuring proper stomach acid production. This is huge for good digestion and sadly many people are on medications that block this extremely important aspect of the process. We need stomach acid – we just need it to be in its proper place.
- Boosting digestive enzymes – along with the above steps, bringing in some supplemental enzymes can help to actually make sure she is breaking down her food well.
- Ensuring fats are being broken down well
- Potentially killing off bad bacteria that might be hanging around through some targeted anti-microbials
- Bringing in friendly bacteria in a way that will help and not add fuel to the fire
It may seem easier to just take something to make the constipation go away, and that can be a part of this process (my favorite is magnesium glycinate → check out my magnesium options on Fullscript), but if you are interested in helping your overall health or also getting rid of seemingly unrelated symptoms, then I recommend a more whole-body approach.
Do you struggle with IBS symptoms? I’d love to chat about how you might be able to find relief. Sign up here for a free, no strings attached phone consultation.
Hi! 🙂 Is it Okay if I ask something kinda off subject? I’m trying to view this web page on my new iPad nevertheless it will not exhibit up correctly, do you’ve any alternatives? Must I try and locate an update for my software program or anything? Thanks upfront! Jennine x 🙂
Like SAP Business One, also MARIProject is utilized in greater than 42 nations.
The consumer has workplaces throughout the UK and the EMEA area, and the role
is hybrid with on-site work of their London headquarters.
With over 15 years of expertise implementing SAP ERP for businesses in Vietnam.
In 2001, SAP made the acquisition that marked its entry into
the small enterprise space.
Beehexa makes use of cutting-edge applied sciences
and optimizations to offer you Hexasync, as an integration Platform as
a Service .
The following 9 certification tracks lie exterior our chosen areas of
expertise and are included for unbiased study on the present time.